(Original article written for Rehab Guru)
“We are at a unique juncture in the history of medicine, with the convergence of genomics, biosensors, the electronic patient record and smartphone apps, all superimposed on a digital infrastructure, with artificial intelligence to make sense of the overwhelming amount of data created. This remarkably powerful set of information technologies provides the capacity to understand, from a medical standpoint, the uniqueness of each individual – and the promise to deliver healthcare on a far more rational, efficient and tailored basis.”
Eric Topol, MD. The Topol Review. Preparing the healthcare workforce to deliver the digital future – An independent report on behalf of the Secretary of State for Health and Social Care February 2019.
This report was published just before the first Lockdown when the true importance of telehealth, providing care at distance, and digitally support self-care was not really understood by the health and care community. At this time there was resistance to new digital technologies, an NHS ladened with debt that did not have sufficient budgets to horizon scan and implement digital transformation at scale, and a workforce that was wary of the impact that digital technologies could have on jobs and personal freedom.
The pandemic, working from home and providing care at distance has created a new appetite for digital technology. The speed of implementation of GP telehealth that occurred in 2019 could not have been dreamt of in 2018 when there was still debate over data security, patients’ technological capabilities, obstacles to interfacing with Electronic Patient Records (EPR), and a paternalistic approach to patient care which led to the belief that all consultations needed to be conducted face-to-face.
Impacts on Patients
The impact on patients of face-to-face consultations in outpatient departments has been a topic that I have been discussing with clinicians for several years, when considering options for digital transformation.
“The ability of digital technologies to streamline access to services and reduce the number of unnecessary visits by patients to hospitals or GP surgeries cannot be overstated. Avoiding just one hospital outpatient appointment has been estimated to save the patient on average £36 in time and travel costs, while similar figures for a primary care appointment are on average £17 per patient. The burden of these costs is disproportionately carried by those least able to afford them”. Topol
I would add to this, if the patient is elderly, frail, or physically unable to get themselves to the appointment the financial impact is then multiplied by the number of friends and family who need to come with them, and potentially take time off work.
Prior to March 2019 it was assumed that older patients would not be able to engage with digital health, use telehealth for consultations, or apps for supportive self-care and treatment. However, we all know that necessity is the mother of invention, and in this case of implementation (many of the digital solutions adopted through the pandemic had existed for some time).
Having conducted multiple interviews across the Dementia Care community during the pandemic, there has been a vivid demonstration of the ability and appetite for patients to use digital technologies. Examples of telehealth consultations between GPs and patients in their 90s who have never experienced video calling, conducting telehealth consultations smoothly without incident. Community Dementia Cafes running online sessions and “radio shows”. One of my interviews was with an expert patient living with dementia who uses video calling and digital health daily, along with helping others in her community. Only through this extreme circumstance has the assumption of patient resistance and inability to engage been disproven.
Rehab Guru and Digital Adoption in the NHS
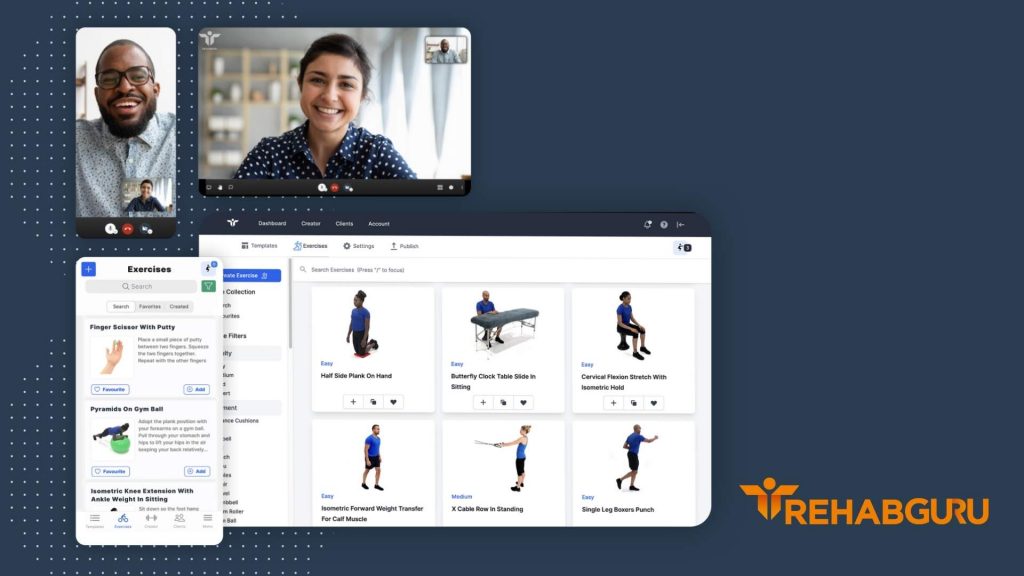
Through the pandemic Rehab Guru has seen a significant increase in enquiries and new clients across the NHS and private sectors. Rehabilitation, MSK, physiotherapy, occupational health and podiatry still need to deliver services to patients, whilst reducing the risk of COVID-19 infection which is present when bringing patients into hospitals and clinics.
Rehab Guru has been seen as a facilitator of care at distance. Not only allowing patients to feel that they are receiving personalised care, but that the support is ongoing, and self-care advice is constantly at hand to provide reassurance.
Home Exercise Prescribing (HEP) has been a significant part of rehabilitation for generations, digitisation is relatively new, and many NHS professionals have limited or no access.
Digital Home Exercise Prescribing, allows for images or videos of exercises to be sent to patients in a digital format. Rehab Guru has one of (if not the) largest video exercise libraries in the world, with over 270 configurable templates of groups of exercises for common conditions to make prescribing quicker and easier. The pandemic has seen a rise in the demand for clinical services to support the acute needs of COVID-19 patients, this has drawn heavily on physiotherapy resources, leaving less time for chronic and rehabilitating patients. Waiting lists are growing.
Already validated by four year’s provision to the Ministry of Defence, and as a provider to The British Association of Sports Rehabilitators and Trainers, and being the digital enabler Healthshare services across 25 CCGs and 27 prisons, Rehab Guru has been approached by a number of NHS Trusts to help them find a solution to the need to treat their physiotherapy patients at distance.
The Problem
- Growing waiting lists, reduced staff availability
- Need to reduce risk of infection, especially for vulnerable patients
- Need to track outcomes
- Team working across wide geographies and clinical specialities
- Share best practice
The Solution
- Patients can be seen in any location, using our clinician app or online platform on any device, in person or virtually, reducing missed appointments and travel times. Staff can work from home and consult with patients if shielding.
- Exercises and templates for respiratory patients
- Working with UCL to develop “Return to fitness after covid” program
- Virtual appointments, digital transfer of information – no risk of pathogen transfers
- Tracking outcomes through the free patient app and monitoring department activity through the digital dashboard
- Options to share records, giving access to prescribed exercise videos to whichever health or care professional is with the patient, for holistic person-centred care
- Standard policies and procedures can be loaded into the platform to be accessible across the whole team
Rehab Guru has been adopted three additional NHS trusts since March 2019, is currently piloting in four North West NHS Trusts, extending to 10, to address the question “Is a digital solution more effective than face-to-face appointments”, supporting work with Imperial College Healthcare NHS FT for a program “Return to activity after Covid”, and is working with NHS Grampian in a collaborative approach to exercise provision for people with Parkinson’s disease.
Experience of highly secure, rapid deployment, at scale means that implementation at scale and speed is not a problem, and the Rehab Guru team can respond to NHS needs flexibly and safely.
If you are seeking to solve similar problems contact them to discuss how they can help you solve them.



